Services
Acute trauma surgery
The dental specialist performs the proper treatment of facial injuries. These professionals must be well versed in emergency care, acute treatment and long-term reconstruction and rehabilitation – not just for physical reasons but emotional as well. Oral and maxillofacial surgeons are trained, skilled and uniquely qualified to manage and treat facial trauma. Injuries to the face, by their very nature, impart a high degree of emotional, as well as physical trauma to patients. The science and art of treating these injuries requires special training involving a “hands on” experience and an understanding of how the treatment provided will influence the patient's long term function and appearance.
Dr. Slavin meets and exceeds these modern standards. He is trained, skilled, and uniquely qualified to manage and treat facial trauma. He is on staff at local hospitals and delivers emergency room coverage for facial injuries, which include the following conditions:
The Nature Of Maxillofacial Trauma
There are a number of possible causes of facial trauma such as motor vehicle accidents, accidental falls, sports injuries, interpersonal violence, and work-related injuries. Types of facial injuries can range from injuries of teeth to extremely severe injuries of the skin and bones of the face. Typically, facial injuries are classified as either soft tissue injuries (skin and gums), bone injuries (fractures), or injuries to special regions (such as the eyes, facial nerves or the salivary glands).
Soft Tissue Injuries Of The Maxillofacial Region
When soft tissue injuries such as lacerations occur on the face, they are repaired by suturing. In addition to the obvious concern of providing a repair that yields the best cosmetic result possible, care is taken to inspect for and treat injuries to structures such as facial nerves, salivary glands, and salivary ducts (or outflow channels). Dr. Slavin is a well-trained oral and maxillofacial surgeon and is proficient at diagnosing and treating all types of facial lacerations.
Bone Injuries Of The Maxillofacial Region
Fractures of the bones of the face are treated in a manner similar to the fractures in other parts of the body. The specific form of treatment is determined by various factors, which include the location of the fracture, the severity of the fracture, the age, and general health of the patient. When an arm or a leg is fractured, a cast is often applied to stabilize the bone to allow for proper healing. Since a cast cannot be placed on the face, other means have been developed to stabilize facial fractures.
One of these options involves wiring the jaws together for certain fractures of the upper and/or lower jaw. Certain other types of fractures of the jaw are best treated and stabilized by the surgical placement of small plates and screws at the involved site. This technique of treatment can often allow for healing and obviates the necessity of having the jaws wired together. This technique is called "rigid fixation" of a fracture. The relatively recent development and use of rigid fixation has profoundly improved the recovery period for many patients, allowing them to return to normal function more quickly.
The treatment of facial fractures should be accomplished in a thorough and predictable manner. More importantly, the patient's facial appearance should be minimally affected. An attempt at accessing the facial bones through the fewest incisions necessary is always made. At the same time, the incisions that become necessary, are designed to be small and, whenever possible, are placed so that the resultant scar is hidden.
Injuries To The Teeth & Surrounding Dental Structures
Isolated injuries to teeth are quite common and may require the expertise of various dental specialists. Oral surgeons usually are involved in treating fractures in the supporting bone or in replanting teeth that have been displaced or knocked out. These types of injuries are treated by one of a number of forms of splinting (stabilizing by wiring or bonding teeth together). If a tooth is knocked out, it should be placed in salt water or milk. The sooner the tooth is re-inserted into the dental socket, the better chance it will survive. Therefore, the patient should see a dentist or oral surgeon as soon as possible. Never attempt to wipe the tooth off, since remnants of the ligament that hold the tooth in the jaw are attached and are vital to the success of replanting the tooth. Other dental specialists may be called upon such as endodontists, who may be asked to perform root canal therapy, and/or restorative dentists who may need to repair or rebuild fractured teeth. In the event that injured teeth cannot be saved or repaired, dental implants are often now utilized as replacements for missing teeth.
The proper treatment of facial injuries is now the realm of specialists who are well versed in emergency care, acute treatment, long-term reconstruction, and rehabilitation of the patient.
anatomical modeling
Dental patient education is vital for the health of our patients and therefore it is important to be able to explain the procedures that will help our patient One of the most effective ways to educate, is with the use of visual aids such as anatomical models and wall charts featuring dental anatomy. As the old saying goes, "a picture is worth a thousand words."
Pointing to relevant dental anatomy on a wall chart or handing you a model that you can see and touch is probably the best way to get the point across. Educated patients are better able to understand and comply with care recommendations, more likely to have greater dental health and more likely to understand that your healing and improvement is a team effort! We are here to help you every way we can.
Bone Grafting
What is a bone graft?
Bone grafting is the replacement or augmentation of the bone around the teeth.
Why is a bone graft needed?Bone grafting is performed to reverse the bone loss / destruction caused by periodontal disease, trauma, or ill fitting removable dentures. It is also used to augment bone to permit implant placement, such as augmenting bone in the sinus area for implant placement, or augmenting bone to enhance the fit and comfort of removable prostheses, or to enhance esthetics of a missing tooth site in the smile zone. When one loses a tooth, as in an extraction, the surrounding bone collapses. To preserve this bone for future implant placement or for esthetics, a bone graft is used. |
Click watch Bone Grafting Procedure |
What are the types of bone graft?1. autogenous - bone taken from one area of the patient and transplanted to another area requiring such grafting
|
Click picture to see tooth extractions that eliminate bone loss |
Allografts and Xenografts both do not require a second surgical site as does the autogenous bone. Ample amounts can be easily obtained.
Barrier membranes - Guided Tissue Regeneration
In conjunction with bone grafting, membranes are often used to help stabilize the bone graft as well as displace the gum tissue from invading the healing bone graft. Gum tissue grows at a much faster rate than bone, therefore, membranes are used to prevent gum tissue from growing in and displacing the bone graft before it matures.
What are the types of bone graft?
1. autogenous - bone taken from one area of the patient and transplanted to another area requiring such grafting
2. allograft - either synthetic bone or bone from a bone bank (cadaver bone)
3. xenograft - bovine /cow bone
Which graft is used and when and why?
Autogenous bone is the "gold standard" and oftentimes has the most predictable results. This is described as the best type of graft because such bone is live bone with live active cellular elements that enhance bone growth, whereas other types of grafts are devoid of any active cellular material.
Allografts and Xenografts both do not require a second surgical site as does the autogenous bone. Ample amounts can be easily obtained.
Barrier membranes - Guided Tissue Regeneration
In conjunction with bone grafting, membranes are often used to help stabilize the bone graft as well as displace the gum tissue from invading the healing bone graft. Gum tissue grows at a much faster rate than bone, therefore, membranes are used to prevent gum tissue from growing in and displacing the bone graft before it matures.
dental implants
Did you know that dental implants are frequently the best treatment option for replacing missing teeth? Rather than resting on the gum line like removable dentures, or using adjacent teeth as anchors like fixed bridges, dental implants are long-term replacements that your oral and maxillofacial surgeon surgically places in the jawbone.
A Solution of Choice for Replacing Missing Teeth
Statistics show that 69% of adults ages 35 to 44 have lost at least one permanent tooth to an accident, gum disease, a failed root canal or tooth decay. Furthermore, by age 74, 26% of adults have lost all of their permanent teeth.
Twenty years ago, these patients would have had no alternative but to employ a fixed bridge or removable denture to restore their ability to eat, speak clearly and smile. Fixed bridges and removable dentures, however, are not the perfect solution and often bring with them a number of other problems. Removable dentures may slip or cause embarrassing clicking sounds while eating or speaking. Of even greater concern, fixed bridges often affect adjacent healthy teeth, and removable dentures may lead to bone loss in the area where the tooth or teeth are missing. Recurrent decay, periodontal (gum) disease and other factors often doom fixed bridgework to early failure. For these reasons, fixed bridges and removable dentures usually need to be replaced every seven to 15 years.


Before (left) and after (right) a dental implant
Today there is another option for patients who are missing permanent teeth. Rather than resting on the gum line like removable dentures, or using adjacent teeth as anchors like fixed bridges, dental implants are long-term replacements that your oral and maxillofacial surgeon surgically places in the jawbone. Composed of titanium metal that "fuses" with the jawbone through a process called "osseointegration," dental implants never slip or make embarrassing noises that advertise the fact that you have "false teeth," and never decay like teeth anchoring fixed bridges. Because dental implants fuse with the jawbone, bone loss is generally not a problem.
After more than 20 years of service, the vast majority of dental implants first placed by oral and maxillofacial surgeons in the United States continue to still function at peak performance. More importantly, the recipients of those early dental implants are still satisfied they made the right choice. If properly cared for, dental implants can last a lifetime.
Anatomy of a Dental Implant
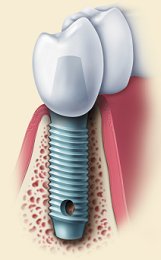 |
A dental implant designed to replace a single tooth is composed of three parts: the titanium implant that fuses with the jawbone; the abutment, which fits over the portion of the implant that protrudes from the gum line; and the crown, which is created by a prosthodontist or restorative dentist and fitted onto the abutment for a natural appearance. |
|
|
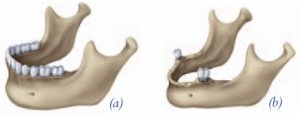
Further, conventional dentures may contribute to the loss of bone in the area where teeth are missing. As illustration (a) indicates, the presence of natural teeth preserves the jawbone. When a tooth is missing, as in illustration (b), the bone may erode and weaken until it may be necessary for your oral and maxillofacial surgeon to graft bone to the area to strengthen it for placement of a dental implant. When a missing tooth is replaced by a dental implant, the fusion, or osseointegration, of the implant and bone provides stability, just as the natural tooth did.
If you are missing several teeth in the same area of your mouth, you may still enjoy the confidence and lifestyle benefits that come with dental implants. Your oral and maxillofacial surgeon will place two or more dental implants, depending on the number of teeth that are missing. Your replacement teeth will be attached to the implants to allow excellent function and prevent bone loss. The implants will serve as a stable support that tightly locks into your replacement teeth and dentures to prevent slipping and bone loss.
With an overall success rate of about 95% and almost 50 years of clinical research to back them up, dental implants are frequently the best treatment option for replacing missing teeth.
Dental Implants vs. Conventional Dentures
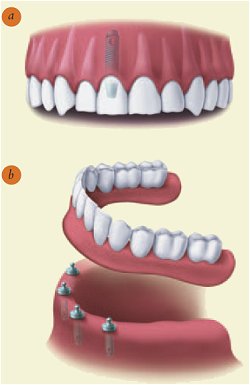 |
Implants can be used to replace one missing tooth so that the replacement looks and feels natural (a). Also, two or more implants can serve as a stable support for the replacement of many teeth (b). |
Dental Implants are a Team Effort
Dental implants combine the best of modern science and technology, including a team approach spanning several disciplines.
A successful implant requires that all parties involved — the patient; the restorative dentist, who makes the crown for the implant; and the oral and maxillofacial surgeon, who surgically places the implant, follow a careful plan of treatment. All members of the implant team stay in close contact with each other to make sure everyone clearly understands what needs to be done to meet the patient's expectations.
The team is organized as soon as the decision for placing a dental implant is reached. Following an evaluation that includes a comprehensive examination, x-rays and a consultation with the patient and members of the implant team, the oral and maxillofacial surgeon surgically places the posts, or implants, in the patient's jaw.
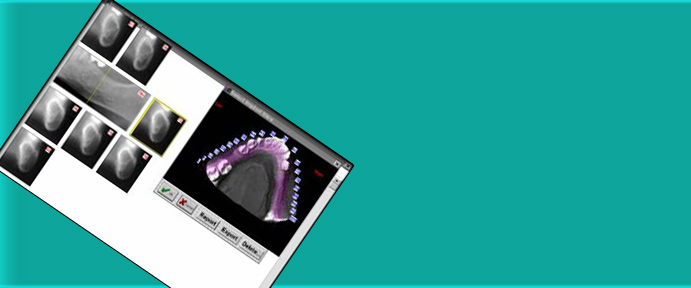
When the implants have stabilized in the jaw, the restorative dentist prepares an impression of the upper and lower jaws. This impression is used to make the model from which the dentures or crowns are created.
The teamwork continues long after the implant and crown have been placed. Follow-up examinations with the oral and maxillofacial surgeon and restorative dentist are critical, and progress is carefully charted. Both the oral and maxillofacial surgeon and the restorative dentist continue to work together to provide the highest level of aftercare.
Are You a Candidate for Dental Implants?
Whether you are a young, middle-aged or older adult; whether you need to replace one tooth, several teeth, or all your teeth, there is a dental implant solution for you. With the exception of growing children, dental implants are the solution of choice for people of all ages, even those with the following health concerns:
Existing Medical Conditions. If you can have routine dental treatment, you can generally have an implant placed. While precautions are advisable for certain conditions, patients with such chronic diseases as high blood pressure and diabetes are usually successful candidates for dental implant treatment.
Gum Disease or Problem Teeth. Almost all implants placed in patients who have lost their teeth to periodontal disease or decay have been successful.
Currently Wearing Partials or Dentures. Implants can replace removable bridges or dentures, or they can be used to stabilize and secure the denture, making it much more comfortable.
Smokers. Although smoking lowers the success rate of implants, it doesn't eliminate the possibility of getting them.
Bone Loss. Bone loss is not uncommon for people who have lost teeth or had periodontal disease. Oral and maxillofacial surgeons are trained and experienced in grafting bone to safely and permanently secure the implant.
Implant tooth replacement in children is usually deferred until their jaw growth is complete. There are, however, some instances when a dental implant may be appropriate, such as when it is part of the child's orthodontic treatment plan. Your family dentist or orthodontist can guide you in this instance.
facial reconstruction
Facts on Facial Reconstruction
Facial reconstruction or Orthognathic Surgery is a surgical procedure or series of procedures performed to rebuild the face of a patient who is either born with physical defects, has abnormal or assymetric jaw development, or suffers an injury or deformity later in life. Performed by an experienced and highly-trained oral and maxillofacial surgeon, facial reconstruction can dramatically improve day-to-day functions of the face and mouth, such as eating and speaking, as well as boost self-esteem by providing a balanced and attractive facial appearance.
Why have Facial Reconstruction?
In some cases, a facial injury or deformity does not impact a patient’s functioning, but he or she may choose to undergo surgery solely for aesthetic reasons. In other instances, the impact on a person’s emotional and physical health is so severe that surgery is necessary to lead a normal life. The following are common indications for facial reconstruction:
Birth Defects or Facial Deformities: Cleft lip and cleft palate are birth defects that are commonly treated by oral surgeons.
Developmental Deformities are perhaps the most common jaw size abnormalities. They are caused by a disproportional growth relationship between the upper and lower jaws resulting in skeletal bite abnormalities. They are often discovered during the teenage years by the dentist or the orthodontist. Orthognathic Surgery is necessary to correct these abnormalities to improve or normalize the jaws and the bite.
Tumors or Deformities Caused by the Removal of Tumors: Growths on the skin or facial bones can distort the appearance of the face, and the surgical procedures used to remove these tumors can also cause disfigurement that needs to be corrected.
Traumatic Injuries: Broken bones and soft tissue injuries to the face can produce excessive scarring and asymmetry that requires reconstruction.
What you would expect with Reconstructive Surgery
Depending on the type of facial injury or deformity, surgery to reconstruct the face can involve a number of techniques. Performed under general anesthesia, facial reconstruction often involves intricate microscopic surgical procedures to protect the blood vessels and nerves of the face while moving and reshaping the bones and soft tissues for a good cosmetic effect. Bone and skin grafts may also be used to rebuild tissues, and bones may be wired in place to ensure stability while they are healing.
While healing times vary, most patients can expect full healing from surgery within about six weeks.
Dr. Slavin provides compassionate care from an experienced oral and maxillofacial surgeon. Injuries and deformities of the face can dramatically reduce your quality of life but we are here to help you. Call for a surgical consultation today.
Anesthesia & Sedation
A child wonders what the first day of school will be like. Someone is about to start a new job. A young couple is about to be married.
Each of these situations is a classic anxiety producer. What they have in common is that each involves the unknown. And that's what anxiety is: the fear of a specific upcoming event that, in all likelihood, you've never before experienced.
The Less You Worry, the Easier it Will Be
An upcoming visit to an Oral and Maxillofacial Surgeon is another potential anxiety producer. In this case, the patient is typically most concerned about possible pain — whether the procedure is going to hurt.
The good news is that whether your procedure requires local or intravenous anesthesia, today's technology makes it possible to perform complex surgery in the oral and maxillofacial surgery office with little or no discomfort for the patient. Knowing this should start to reduce your level of anxiety.
Extensive Training and Experience in the Control of Pain and Anxiety
The ability to provide patients with safe, effective outpatient anesthesia has distinguished the specialty of oral and maxillofacial surgery since its earliest days. As the surgical specialists of the dental profession, Oral and Maxillofacial Surgeons are trained in all aspects of anesthesia administration. Following dental school, Oral and Maxillofacial Surgeons complete at least four years of training in a hospital-based surgical residency program alongside medical residents in general surgery, anesthesia and other specialties. During this time, OMS residents must complete a rotation on the medical anesthesiology service, during which they become competent in evaluating patients for anesthesia, delivering the anesthetic and monitoring post-anesthetic patients.
As a result of this extensive training, Oral and Maxillofacial Surgeons are well-prepared to identify, diagnose and assess the source of pain and anxiety within the scope of their discipline, and to appropriately administer local anesthesia, all forms of sedation and general anesthesia. Further, they are experienced in airway management, endotracheal intubation, establishing and maintaining intravenous lines, and managing complications and emergencies that may arise during the administration of anesthesia.
Putting Your Mind at Ease
The best way to reduce anxiety is to make certain you know what to expect during and after surgery. As with most anxiety-producing situations, the more you know, the less you have to be anxious about. Prior to surgery, your Oral and Maxillofacial Surgeon will review with you the type of anesthetic to be used, as well as the way you're likely to feel during and after the operation.This is the time to discuss any concerns you may have about any facet of the operation.
During surgery, one or more of the following may be used to control your pain and anxiety: local anesthesia, nitrous oxide-oxygen, intravenous sedation and general anesthesia. Commonly, patients describe their feelings during surgery as comfortable and surprisingly pleasant.
After surgery, you may be prescribed a medication to make you as comfortable as possible when you get home.
Jaw Surgery
Corrective jaw, or orthognathic, surgery is performed by Oral and Maxillofacial Surgeons to correct a wide range of minor and major skeletal and dental irregularities, including the misalignment of jaws and teeth, which, in turn, can improve chewing, speaking and breathing. While the patient's appearance may be dramatically enhanced as a result of their surgery, orthognathic surgery is performed to correct functional problems.
Following are some of the conditions that may indicate the need for corrective jaw surgery:
difficulty chewing, or biting food
difficulty swallowing
chronic jaw or jaw joint (TMJ) pain and headache
excessive wear of the teeth
open bite (space between the upper and lower teeth when the mouth is closed)
unbalanced facial appearance from the front, or side
facial injury or birth defects
receding chin
protruding jaw
inability to make the lips meet without straining
chronic mouth breathing and dry mouth
sleep apnea (breathing problems when sleeping, including snoring)
Who Needs Corrective Jaw Surgery?
People who may benefit from corrective jaw surgery include those with an improper bite resulting from misaligned teeth and/or jaws. In some cases, the upper and lower jaws may grow at different rates. Injuries and birth defects may also affect jaw alignment. While orthodontics can usually correct bite, or "occlusion," problems when only the teeth are misaligned, corrective jaw surgery may be necessary to correct misalignment of the jaws.
Evaluating Your Need for Corrective Jaw Surgery
Your dentist, orthodontist and Oral and Maxillofacial Surgeon will work together to determine whether you are a candidate for corrective jaw, or orthognathic, surgery. The Oral and Maxillofacial Surgeon determines which corrective jaw surgical procedure is appropriate and performs the actual surgery. It is important to understand that your treatment, which will probably include orthodontics before and after surgery, may take several years to complete. Your Oral and Maxillofacial Surgeon and orthodontist understand that this is a long-term commitment for you and your family.They will try to realistically estimate the time required for your treatment.
Corrective jaw surgery may reposition all or part of the upper jaw, lower jaw and chin. When you are fully informed about your case and your treatment options, you and your dental team will determine the course of treatment that is best for you.
Correction of Common Dentofacial Deformities
Correcting an Open Bite: Some of the bone in the upper tooth-bearing portion of the jaw is removed. The upper jaw is then secured in position with plates and screws.
Correcting a Protruding Lower Jaw: The bone in the rear portion of the jaw is separated from the front portion and modified so that the tooth-bearing portion of the lower jaw can be moved back for proper alignment.
Correcting a Receding Lower Jaw or "Weak Chin": The bone in the lower portion of the jaw is separated from its base and modified. The tooth-bearing portion of the lower jaw and a portion of the chin are repositioned forward.
What Is Involved in Corrective Jaw Surgery?
Before your surgery, orthodontic braces move the teeth into a new position. Because your teeth are being moved into a position that will fit together after surgery, you may at first think your bite is getting worse rather than better. When your Oral and Maxillofacial Surgeon repositions your jaws during surgery, however, your teeth should fit together properly.
As your pre-surgical orthodontic treatment nears completion, additional or updated records, including x-rays, pictures and models of your teeth, may be taken to help guide your surgery.
Depending on the procedure, corrective jaw surgery may be performed under general anesthesia in a hospital, an ambulatory surgical center or in the oral and maxillofacial surgery office. Surgery may take from one to several hours to complete.
Your Oral and Maxillofacial Surgeon will reposition the jawbones in accordance with your specific needs. In some cases, bone may be added, taken away or reshaped. Surgical plates, screws, wires and rubber bands may be used to hold your jaws in their new positions. Incisions are usually made inside the mouth to reduce visible scarring; however, some cases do require small incisions outside of the mouth. When this is necessary, care is taken to minimize their appearance.
After surgery, your surgeon will provide instructions for a modified diet, which may include solids and liquids, as well as a schedule for transitioning to a normal diet. You may also be asked to refrain from using tobacco products and avoid strenuous physical activity.
Pain following corrective jaw surgery is easily controlled with medication and patients are generally able to return to work or school from one to three weeks after surgery, depending on how they are feeling. While the initial healing phase is about six weeks, complete healing of the jaws takes between nine and 12 months.
Oral Pathology
The inside of the mouth is normally lined with a special type of skin (mucosa) that is smooth and coral pink in color. Any alteration in this appearance could be a warning sign for a pathological process. The most serious of these is oral cancer. The following can be signs at the beginning of a pathologic process or cancerous growth.
Reddish patches (erythroplasia) or whitish patches (leukoplakia) in the mouth
A sore that fails to heal and bleeds easily
A lump or thickening on the skin lining the inside of the mouth
Chronic sore throat or hoarseness
Difficulty in chewing or swallowing
These changes can be detected on the lips, cheeks, palate and gum tissue around the teeth, tongue, face and/or neck. Pain does not always occur with pathology, and curiously, is not often associated with oral cancer. However, any patient with facial and/or oral pain without an obvious cause or reason may also be at risk for oral cancer.
We would recommend performing an oral cancer self-examination monthly and remember that your mouth is one of your body's most important warning systems. Do not ignore suspicious lumps or sores. Please contact us so we may help.
Oral SEDATION
What Is Sedation Dentistry?
Sedation dentistry uses medication to help patients relax during dental procedures. It's sometimes referred to as "sleep dentistry," although that's not entirely accurate. Patients are usually awake with the exception of those who are under general anesthesia.
The levels of sedation used include:
Minimal sedation -- you are awake but relaxed.
Moderate sedation (formerly called "conscious sedation") -- You may slur your words when speaking and not remember much of the procedure.
Deep sedation -- you are on the edge of consciousness but can still be awakened.
General anesthesia -- you are completely unconscious.
Who Can Have Sedation at the Dentist's?
Sedation is most appropriate for people with a real fear or anxiety that is preventing them from going to the dentist.
Sedation dentistry may also be appropriate for people who:
have a low pain threshold
can't sit still in the dentist's chair
have very sensitive teeth
have a bad gag reflex
need a large amount of dental work completed
Sometimes, children are given sedation if they are terrified of going to the dentist or refuse to cooperate during the visit. Nitrous oxide tends to be safe in children, and just about any dentist can administer it. A smaller percentage of pediatric dentists are trained to give children oral sedation. Oral sedation can be safe when kept within the recommended dose for the child's age and weight.
Can Any Dentist Perform Sedation?
Most dentists can administer minimal sedation (such as nitrous oxide or pills). An increasing number of dentists can give moderate sedation. However, only a small percentage of dentists who have completed the Commission on Dental Accreditation (CODA) program in deep sedation and general anesthesia can use these more complex techniques. These dentists are typically oral and maxillofacial surgeons and dentist anesthesiologists. Some dentists use a dentist anesthesiologist, who is specially trained to give all levels of sedation and anesthesia to both children and adults.
Each state's dental board carefully regulates the use of sedation techniques. Many states require dentists to hold permits in order to perform sedation.
How Safe Is Sedation Dentistry?
There is always a risk in getting anesthesia. It is usually safe, though, when given by experienced dentists. However, certain people, such as those who are obese or who have obstructive sleep apnea, should talk to their doctor before having sedation. That's because they are more likely to develop complications from the anesthesia.
It's important to make sure that your dentist is trained and qualified to administer the type of sedation you will be receiving. To be a smart patient, you should make sure the following things are done:
Before the procedure, your dentist should go over your medical history. Your dentist should also determine whether you are an appropriate candidate for sedation and ask about any medications you're currently taking.
You should ask what dose of the sedative is appropriate for your age and health. You should also ask whether it is within the dose recommended by the FDA.
It's important to find out how much training the dentist has and how many procedures he or she has performed using sedation. The more procedures the dentist has performed, the better.
You should receive a form detailing the risks of the procedure. Go over it carefully with your dentist. Ask questions if you're unclear on any of the wording.
The dentist should monitor your vital signs during the procedure following the American Dental Association's guidelines. The dentist should also have oxygen -- artificial ventilation -- and drugs that reverse the effects of sedation on hand in case you need them.
Corrective Jaw Surgery / Orthognathic
Corrective jaw, or orthognathic, surgery is performed by Oral and Maxillofacial Surgeons to correct a wide range of minor and major skeletal and dental irregularities, including the misalignment of jaws and teeth, which, in turn, can improve chewing, speaking and breathing. While the patient's appearance may be dramatically enhanced as a result of their surgery, orthognathic surgery is performed to correct functional problems.
Following are some of the conditions that may indicate the need for corrective jaw surgery:
difficulty chewing, or biting food
difficulty swallowing
chronic jaw or jaw joint (TMJ) pain and headache
excessive wear of the teeth
open bite (space between the upper and lower teeth when the mouth is closed)
unbalanced facial appearance from the front, or side
facial injury or birth defects
receding chin
protruding jaw
inability to make the lips meet without straining
chronic mouth breathing and dry mouth
sleep apnea (breathing problems when sleeping, including snoring)
Who Needs Corrective Jaw Surgery?
People who may benefit from corrective jaw surgery include those with an improper bite resulting from misaligned teeth and/or jaws. In some cases, the upper and lower jaws may grow at different rates. Injuries and birth defects may also affect jaw alignment. While orthodontics can usually correct bite, or "occlusion," problems when only the teeth are misaligned, corrective jaw surgery may be necessary to correct misalignment of the jaws.
Evaluating Your Need for Corrective Jaw Surgery
Your dentist, orthodontist and Oral and Maxillofacial Surgeon will work together to determine whether you are a candidate for corrective jaw, or orthognathic, surgery. The Oral and Maxillofacial Surgeon determines which corrective jaw surgical procedure is appropriate and performs the actual surgery. It is important to understand that your treatment, which will probably include orthodontics before and after surgery, may take several years to complete. Your Oral and Maxillofacial Surgeon and orthodontist understand that this is a long-term commitment for you and your family.They will try to realistically estimate the time required for your treatment.
Corrective jaw surgery may reposition all or part of the upper jaw, lower jaw and chin. When you are fully informed about your case and your treatment options, you and your dental team will determine the course of treatment that is best for you.
Correction of Common Dentofacial Deformities
Correcting an Open Bite: Some of the bone in the upper tooth-bearing portion of the jaw is removed. The upper jaw is then secured in position with plates and screws.
Correcting a Protruding Lower Jaw: The bone in the rear portion of the jaw is separated from the front portion and modified so that the tooth-bearing portion of the lower jaw can be moved back for proper alignment.
Correcting a Receding Lower Jaw or "Weak Chin": The bone in the lower portion of the jaw is separated from its base and modified. The tooth-bearing portion of the lower jaw and a portion of the chin are repositioned forward.
What Is Involved in Corrective Jaw Surgery?
Before your surgery, orthodontic braces move the teeth into a new position. Because your teeth are being moved into a position that will fit together after surgery, you may at first think your bite is getting worse rather than better. When your Oral and Maxillofacial Surgeon repositions your jaws during surgery, however, your teeth should fit together properly.
As your pre-surgical orthodontic treatment nears completion, additional or updated records, including x-rays, pictures and models of your teeth, may be taken to help guide your surgery.
Depending on the procedure, corrective jaw surgery may be performed under general anesthesia in a hospital, an ambulatory surgical center or in the oral and maxillofacial surgery office. Surgery may take from one to several hours to complete.
Your Oral and Maxillofacial Surgeon will reposition the jawbones in accordance with your specific needs. In some cases, bone may be added, taken away or reshaped. Surgical plates, screws, wires and rubber bands may be used to hold your jaws in their new positions. Incisions are usually made inside the mouth to reduce visible scarring; however, some cases do require small incisions outside of the mouth. When this is necessary, care is taken to minimize their appearance.
After surgery, your surgeon will provide instructions for a modified diet, which may include solids and liquids, as well as a schedule for transitioning to a normal diet. You may also be asked to refrain from using tobacco products and avoid strenuous physical activity.
Pain following corrective jaw surgery is easily controlled with medication and patients are generally able to return to work or school from one to three weeks after surgery, depending on how they are feeling. While the initial healing phase is about six weeks, complete healing of the jaws takes between nine and 12 months.
Revision trauma surgery
Surgical care of the temporomandibular joint
TMJ revision procedures
Tooth Extraction
TMJ REVISION PROCEDURES
TMJ (temporomandibular joint) disorders are a family of problems related to your complex jaw joint. If you have had symptoms like pain or a "clicking" sound, you'll be glad to know that these problems are more easily diagnosed and treated than they were in the past. These symptoms occur when the joints of the jaw and the chewing muscles (muscles of mastication) do not work together correctly. TMJ stands for temporomandibular joint, which is the name for each joint (right and left) that connects your jaw to your skull. Since some types of TMJ problems can lead to more serious conditions, early detection and treatment are important.
No one treatment can resolve TMJ disorders completely and treatment takes time to become effective.
Dr. Slavin can help you have a healthier and more comfortable jaw.
Trouble With Your Jaw?
TMJ disorders develop for many reasons. You might clench or grind your teeth, tightening your jaw muscles and stressing your TM joint. You may have a damaged jaw joint due to injury or disease. Injuries and arthritis can damage the joint directly or stretch or tear the muscle ligaments. As a result, the disk, which is made of cartilage and functions as the “cushion” of the jaw joint, can slip out of position. Whatever the cause, the results may include a misaligned bite, pain, clicking, or grating noise when you open your mouth or trouble opening your mouth wide.
Do You Have A TMJ Disorder?
Are you aware of grinding or clenching your teeth?
Do you wake up with sore, stiff muscles around your jaws?
Do you have frequent headaches or neck aches?
Does the pain get worse when you clench your teeth?
Does stress make your clenching and pain worse?
Does your jaw click, pop, grate, catch, or lock when you open your mouth?
Is it difficult or painful to open your mouth, eat, or yawn?
Have you ever injured your neck, head, or jaws?
Have you had problems (such as arthritis) with other joints?
Do you have teeth that no longer touch when you bite?
Do your teeth meet differently from time to time?
Is it hard to use your front teeth to bite or tear food?
Are your teeth sensitive, loose, broken or worn?
The more times you answered "yes", the more likely it is that you have a TMJ disorder. Understanding TMJ disorders will also help you understand how they are treated.
Treatment
There are various treatment options that Dr. Slavin can utilize to improve the harmony and function of your jaw. Once an evaluation confirms a diagnosis of TMJ disorder, Dr. Slavin will determine the proper course of treatment. It is important to note that treatment always works best with a team approach of self-care joined with professional care.
The initial goals are to relieve the muscle spasm and joint pain. This is usually accomplished with a pain reliever, anti-inflammatory, or muscle relaxant. Steroids can be injected directly into the joints to reduce pain and inflammation. Self-care treatments can often be effective as well and include:
Resting your jaw
Keeping your teeth apart when you are not swallowing or eating
Eating soft foods
Applying ice and heat
Exercising your jaw
Practicing good posture
Stress management techniques such as biofeedback or physical therapy may also be recommended, as well as a temporary, clear plastic appliance known as a splint. A splint (or nightguard) fits over your top or bottom teeth and helps keep your teeth apart, thereby relaxing the muscles and reducing pain. There are different types of appliances used for different purposes. A nightguard helps you stop clenching or grinding your teeth and reduces muscle tension at night and helps to protect the cartilage and joint surfaces. An anterior positioning appliance moves your jaw forward, relives pressure on parts of your jaw and aids in disk repositioning. It may be worn 24 hours/day to help your jaw heal. An orthotic stabilization appliance is worn 24 hours/day or just at night to move your jaw into proper position. Appliances also help to protect from tooth wear.
What About Bite Correction Or Surgery?
If your TMJ disorder has caused problems with how your teeth fit together, you may need treatment such as bite adjustment (equilibration), orthodontics with or without jaw reconstruction, or restorative dental work. Surgical options such as arthroscopy and open joint repair restructuring are sometimes needed, but are reserved for severe cases. Dr. Slavin does not consider TMJ surgery unless the jaw can’t open, is dislocated and nonreducible, has severe degeneration, or the patient has undergone appliance treatment unsuccessfully.
Tooth Extraction
What to expect during the tooth extraction process.
When your dentist performs the extraction you should expect that you will feel a lot of pressure, here's why.
The root portion of a tooth is firmly encased in bone (its socket) and it is tightly bound into place in this socket by a ligament. During the extraction process the dentist needs to expand the socket (widen and enlarge it) and separate the tooth from its ligament to a point where the tooth is loose and free to come out.
The bone of the jaw is compressible to some degree. That means if a dentist can apply firm pressure to a tooth, forcing it against one of the sides of its socket, the bone in that area will become compressed. The net result is that the socket becomes slightly enlarged. After repeated application of pressure to a tooth, from many different directions, the entire socket becomes larger. The ligament that holds the tooth in place will become detached from the tooth too. Finally at some point, enough space will have been created and the ligament separated from the tooth enough that the tooth will come out.
Dentists have a variety of tools they use to manipulate and apply pressure to teeth. Some of them are specialized pliers termed "extraction forceps." Dentists also use levers that are called "elevators" (they look somewhat similar to small screwdrivers). Usually a dentist will use an elevator first. These tools are intended to wedge between the tooth and the bone surrounding it. The force the dentist applies to the elevator in turn places pressure on the tooth. This action on the tooth helps to expand its socket and separate its ligament. It's somewhat common that a tooth can be extracted with just the use of an elevator.
Understanding the dentist's use of extraction forceps is more straightforward. The dentist will grasp the tooth with the forceps and then firmly and deliberately rock the tooth back and forth. They will also rotate the tooth as much as it will. The combination of these tooth movements expands the tooth's socket and separates its ligament.
Why you will feel pressure, yet no pain, during a tooth extraction.
The reason you will feel pressure during the tooth extraction process is because our bodies have different types of nerve fibers, each of which carry different types of sensations. Each of these different types of nerve fibers have different physical characteristics. The local anesthetic ("novocaine," more actually usually lidocaine) that a dentist uses to "numb up" a tooth is very effective at inhibiting the function of nerve fibers that transmit pain sensations, but it doesn't have as great an effect on the nerves that transmit pressure sensations.
So, expect to feel pressure during the tooth extraction process, even a whole lot of pressure, but don't assume that this indicates that you will soon be feeling pain because it doesn't. If you do find you feel pain (discomfort that has a sharpness to it) during the extraction process, you should let your dentist know so they can "numb you up" some more. But more anesthetic will not reduce the pressure sensation you are experiencing.
You might hear some extraction noises.
It is possible that during a tooth's removal you will hear some of the noises associated with the extraction process. As an example, patients are sometimes concerned that they have heard a snap or breaking noise. In most cases the event that has produced this type of sound is just a minor issue, usually one of the tooth's roots fracturing. Because this "complication" happens so frequently you can anticipate that your dentist has had plenty of experience in removing broken tooth roots.
Gum and bone tissue removal.
Gum and/or bone tissue may cover over or surround a tooth in a manner that makes it difficult for the dentist to view and/or access it. If so, the dentist will need to reflect back or remove this tissue.
Sectioning a tooth during an extraction.
Sometimes a tooth is so firmly anchored in its socket, or else the tooth's roots are so curved, that the dentist can't get the tooth's socket expanded enough that it will come out. In this type of situation one of a dentist's tricks is to cut the tooth into pieces and then remove each portion individually.
Don't be alarmed if your dentist tells you that this technique is required. Sectioning teeth is very commonplace and can significantly reduce the amount of time and effort needed to remove a tooth.
Tumor resection
This content section from MD Anderson Cancer Center
If you are diagnosed with mouth or oropharynx cancer, your doctor will explain your prognosis and treatment options. Your prognosis is what the doctor believes will happen: your chance of recovery, the expected course of the cancer, and how long you might be sick.
Your prognosis takes into consideration the location of the tumor and the stage of the cancer—whether and how far the tumor has spread to nearby tissues, lymph nodes, or other parts of the body. Your options for treatment are determined by the stage and location of the cancer, your age and general health, and whether your appearance and the ability to talk and eat will remain the same after treatment.
Take the time to carefully consider all your treatment options. For many people, a second opinion can help you get more information and decide on the treatment to pursue.
Because the mouth and throat are crucial components of eating, breathing, and talking, a group of healthcare professionals referred to as a multidisciplinary team will probably manage your treatment and rehabilitation. This team will be led by a doctor who specializes in treating people with cancer. This doctor may be a surgeon, radiation oncologist, or medical oncologist. Members of the team include:
Head and neck surgeons, medical oncologists, and radiation oncologists
Plastic and reconstructive surgeons
Dentists
Speech, occupational, and physical therapists
Dietitians
Psychologists
Rehabilitation specialists
This section contains information on:
Staging helps your doctor plan your treatment. It also provides information about the prognosis (expected outcome) of your cancer. Tumor stage is determined by the size of the primary tumor, how much it has invaded the tissues, and whether the cancer has spread to the lymph nodes.
Stage 0
Cancer is "in situ," meaning it is isolated and has not traveled into a deeper layer of tissue or the lymph nodes, small almond-shape glands that help fight infection or trap tumor cells.
Stage I
Tumor is 2 centimeters (about ¾ inch) or smaller.
Tumor has not spread to lymph nodes or other parts of the body.
Stage II
Tumor is between 2 and 4 centimeters (from ¾ to 1½ inches).
Tumor has not spread to lymph nodes or other parts of the body.
Stage III
Tumor is either:
Larger than 4 centimeters (1½ inches) or
Any size and has traveled to one lymph node on the same side of the head or neck. The lymph node with cancer measures 3 centimeters or less.
Tumor has not spread to other parts of the body.
Stage IV
Tumor is any size and has invaded deeply into muscle or facial skin or the jaws and has spread to:
More than one lymph node on the same side of the head or neck as the main tumor
Lymph nodes on one or both sides of the neck
Any lymph node that measures more than 6 centimeters (2½ inches)
Other parts of the body
Recurrent
The mouth and oropharynx cancer has reappeared after it was treated. It may reappear in the oral cavity or another part of the body.
Surgery
Surgery is the most common treatment for mouth cancer, while oropharynx cancer is usually treated with radiation, with or without chemotherapy. Surgery is performed on some patients with cancers of the tonsil and patients with tumor invasion of the jaw. Most salivary gland tumors of the mouth and throat are treated with surgery initially. The type of surgery depends on the type and stage of the cancer. Multiple surgeries may be necessary to treat the cancer and restore function and appearance.
Common types of surgery for mouth and oropharynx cancer include:
Tumor "resection" (removal of the cancerous part of the organ) or a wide local incision to remove the tumor and surrounding noncancerous tissue
Removal of part or all of the jaw
Maxillectomy to remove bone in the roof of the mouth
Neck dissection or removal of lymph nodes and other tissue in the neck
Plastic surgery, including skin grafts, tissue flaps, and dental implants to repair or restore tissues removed from the mouth, throat, or neck
Tracheotomy, or placing a hole in the windpipe, to assist in breathing for patients with very large tumors or after surgical removal of the tumor
Dental surgery to remove teeth or assist with reconstruction
Even if the surgeon removes all the cancer, some patients may need additional treatment to increase the chance of successful outcomes. Those may include chemotherapy or radiation therapy.
Side effects depend on the type of surgery. Possible side effects are:
Pain and discomfort. Discuss pain relief with your doctor before and after the surgery.
Fatigue
Temporary facial swelling
Problems with chewing, swallowing, or talking
Additional surgeries or other therapy may be necessary to address some of these problems.
Radiation therapy
Radiation therapy uses high-energy X-rays or other types of radiation to kill cancer cells or shrink tumors. Chemotherapy can be combined with radiation to increase the cancer-killing effects. In cancer of the mouth and oropharynx, radiation therapy may be used alone to treat small to intermediate-stage tumors or to kill remaining cancerous cells after surgery, or it may be combined with chemotherapy for advanced tumors.
A radiation oncologist, a doctor who specializes in radiation therapy, will give you radiation treatments. This doctor will determine the length of your radiation treatment.
Radiation therapy has a much higher chance of success if you do not use tobacco during treatment.
Since oral side effects are common, any necessary dental care or extractions should be taken care of at least two weeks before the radiation treatment.
External radiation therapy
External radiation therapy is the most common type of radiation used to treat cancers of the mouth and oropharynx. It uses a beam of radiation that is carefully targeted from a machine outside the body. Treatment commonly includes five sessions a week for five to seven weeks.
You will lie on a treatment table, and the radiation therapist will position you so the radiation reaches the correct part of your body. Once you are positioned, you cannot move until the treatment, which takes only a few minutes, is finished. To help you remain still, a custom-fitted plastic head or shoulder mask may be used. Like an X-ray, the procedure is painless. New techniques for delivering external radiation are designed to keep normal tissues safe from the effects of radiation. Known as intensity-modulated radiotherapy, these highly focused beams treat the tumor while sparing salivary gland tissue, thus decreasing the loss of saliva production.
Internal radiation or brachytherapy
In this treatment, radiation is delivered to the body from seeds, needles, or tubes that are implanted into the tumor. After the implants are in place, you will remain in the hospital for several days with limited human contact. The implants will be removed before you leave the hospital.
The method of radiation treatment used depends on the type and stage of cancer. Sometimes both methods are used.
Side effects of radiation treatment may include:
Chemotherapy uses drugs to kill cancer cells or stop them from growing. The drugs can be given by mouth or injected into a vein or muscle. Usually, chemotherapy is given to a patient through a vein during an outpatient visit.
Chemotherapy may be used to shrink the cancer before surgery or radiation, or it may be combined with radiation to increase the effectiveness of both treatments. It may also be used to shrink tumors that cannot be surgically removed.
The most commonly used drugs in mouth and oropharynx cancer are cisplatin and 5-fluorouracil. Carboplatin and paclitaxel are also used in combination.
Chemotherapy affects normal cells as well as cancer cells. You may experience side effects that include:
Discuss any side effects with your doctor. Medication is available to help many of them. Most side effects go away when treatment is complete.
Tumor growth inhibitors
New research on growth factors, hormonelike substances that occur naturally in the body and cause cell growth, shows promise in the treatment of mouth and oropharynx cancer. An epidermal growth factor on the surface of some mouth and oropharynx cancer cells can bind to certain substances that stimulate the tumor to grow. New drugs are being tested that target EGF receptors and may stop cancer cells from growing.
The Food and Drug Administration has approved cetuximab (Erbitux), which blocks the EGF receptor, for use with radiation in people with advanced oral cancer. Other drugs are being studied.
Reconstruction and rehabilitation
After treatment, some patients with mouth and oropharynx cancer may require plastic or reconstructive surgery to restore appearance or function. Grafts of skin, muscle, or bone, which are moved from another part of body to the oral cavity, are often used.
Sometimes it is possible for the surgeon to perform reconstructive surgery at the same time as your cancer surgery; in other cases it is best to wait. Your doctor will tell you which method is right for you.
If surgery to rebuild the mouth cavity cannot be performed, you may be fitted for a dental prosthesis or dental implant. A therapist will show you how to use the device.
Mouth and oropharynx cancer and treatment often cause difficulty in speaking, swallowing, and breathing. After treatment, you may receive therapy and training from various professionals, including dietitians; speech, physical, and occupational therapists; and psychologists.
Wisdom Teeth
Wisdom teeth, also known as third molars, are the last teeth to erupt in your mouth. This generally occurs between the ages of 17 and 25, a time of life that has been called the "Age of Wisdom."
Anthropologists note that the rough diet of early humans resulted in the excessive wear of their teeth. Normal drifting of the teeth to compensate for this wear ensured that space was available for most wisdom teeth to erupt by adolescence. The modern diet, which is much softer, and the popularity of orthodontic tooth straightening procedures produce a fuller dental arch, which quite commonly doesn't leave room for the wisdom teeth to erupt, thereby setting the stage for problems when the final four molars enter the mouth.
What is an Impacted Tooth?
Complications such as infection (fig. a) , damage to adjacent teeth (fig. b) and the formation of cysts (fig. c) may arise from impacted teeth.
|
|
|